Prostate cancer is the most common type of cancer that affects men in the UK, with more than 52,000 men diagnosed a year on average, according to Prostate Cancer UK.
Radical prostatectomy surgery is an effective way to treat men who are eligible, removing the prostate gland to eliminate or control the spread of cancer — but almost 100 per cent of prostatectomy patients experience side effects like bladder incontinence and erectile dysfunction, bearing a huge impact on their day-to-day life as they start the road to recovery.
Stephanie Smith-Rowles, director of Gloucestershire's only men's health physiotherapy clinic Aubergine Physio, speaks to SoGlos about how her clinic can support men in the county who are preparing for and recovering from a prostatectomy.
What do you cover in an initial assessment with someone who is considering a prostatectomy?
Here at Aubergine Physio, we welcome anyone who's had a recent diagnosis of prostate cancer and is looking at having a prostatectomy, rather than radiotherapy, to come along for a consultation to find out how we can support their recovery.
Usually, they'll have a lead time of a month or two before their surgery and organising an initial physiotherapy consultation in this time is key to learning the correct way of strengthening your pelvic floor prior to your operation. This consultation really helps to build a mind-muscle connection, enabling a speedier recovery following on from bladder incontinence after surgery.
Our physiotherapy plans are tailored to each individual so when we first meet a client, we'll get a bit of history — about the diagnosis, how they are currently and what sort of activities they do, so we can recommend appropriate pelvic floor exercises for their lifestyle. Are they picking up young grandkids, for example, or are they into gardening? Will they be doing a lot of digging, bending over, picking things up or will they be under a car doing mechanics?
It's really important to learn how to engage the anterior pelvic floor muscles correctly before the prostate is removed, so this initial assessment is key.
How exactly do pelvic floor exercises help prostate cancer patients in their recovery?
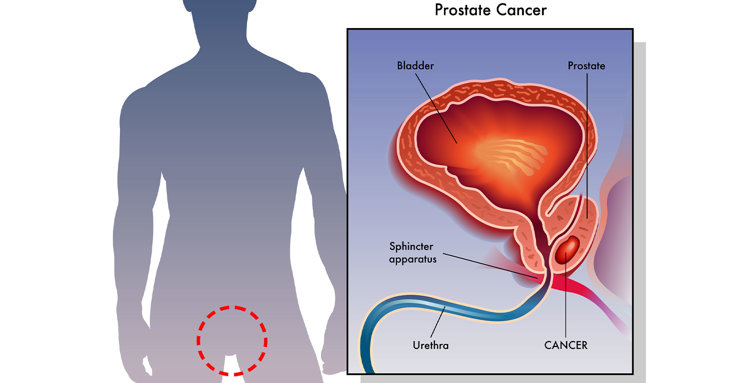
It's difficult for patients to control urine flow and continence after a prostatectomy, because the bladder will rest directly on the pelvic floor without a prostate gland and the internal urethral sphincter is sometimes removed during surgery.
Urinary incontinence post-surgery can last up to 12 weeks, sometimes longer, so establishing a strong mind-muscle connection and working on the pelvic floor for six to eight weeks prior can really help them to manage this.
We teach men to work the front part of their pelvic floor to help with incontinence. The way we teach it is called ‘nuts to guts’ or I sometimes call it ‘balls to belly’ — it's an idea that was designed by an Australian physio called Jo Milios, to encourage men to work the anterior part of the pelvic floor surrounding the urethra. Putting too much focus on the back can create an overactive pelvic floor, and an ineffective control of bladder incontinence, which can sometimes lead to pelvic pain.
We ask them to practice in two ways: to strengthen the slow twitch muscle fibres and the fast twitch muscle fibres.
A slow
twitch contraction is when you engage the
pelvic floor to about 25 to 50 per cent, holding it for as long as you can, working on muscle endurance, for up to a minute
and repeating that process 10 times. A fast twitch
contraction is a maximal 100 per cent, fuller
contraction that engages the pelvic floor strongly
— we recommend men practice this in
preparation for when they're about to pick something up, in short, sharp on/off contractions, so it feels like a short, fast
contraction followed by full relaxation. They should repeat this as many times as they
can within 10 seconds initially, and building up to as many contractions as
they can within a one-minute time frame.
What other side effects can prostatectomy patients expect post-surgery?
As well as bladder incontinence, surgery also affects the nerves around the prostate, which causes erectile dysfunction in 100 per cent of patients.
During a radical prostatectomy, it is sometimes difficult for the surgeon to spare the cavernous nerve bundles that surround the prostate — in this instance, all patients will have erectile dysfunction as a result. For patients whose prostate cancer is less advanced, the surgeon can, in some cases, perform a prostatectomy with nerve sparing surgery — however, the nerves can still be significantly bruised during surgery and this bruising or ‘neuropraxia’ can last for up to a year to 18 months before the nerves fully recover and erectile function returns naturally.
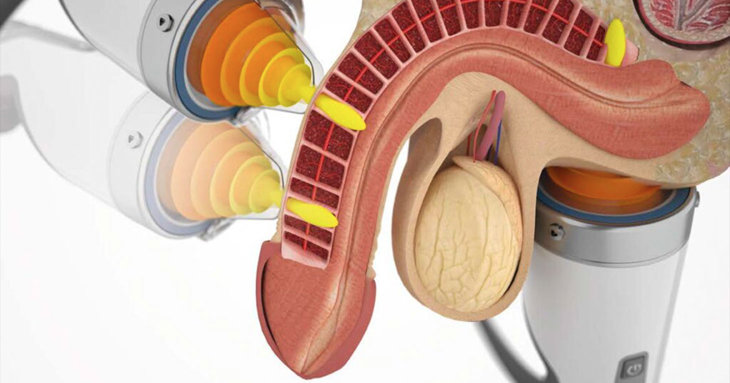
Erectile dysfunction can also be a side effect of high-intensity focused ultrasound (HIFU) treatment for prostate cancer.
How do you treat erectile dysfunction as a side effect of a prostatectomy?
It can take up to a year to 18 months for erections to come back naturally after the operation but at Aubergine Physio, we can provide Focused Shockwave Therapy to help men get their erections back faster.
Focused Shockwave Therapy is a
non-invasive treatment to improve the function of the erection mechanism, using
low-intensity sound waves to stimulate a healing response in the penis, the crura and the cavernosa nerves. It encourages the
development of new collagen within the penile tissue, and can really help to
heal scar tissue, to stimulate new blood vessels and to break
down plaques within the blood vessels. It can also create neurogenesis — new nerves — and help to stimulate and heal the nerves inside the
body.
The treatment can be administered six-weeks post-surgery, if the patient is deemed cancer free by their surgeon and prostate-specific antigen (PSA) levels are negligent. We would usually do around six to 12 sessions.
Because of the damage that's been done to the nerves during a prostatectomy, we can't promise the 70 to 80 per cent success rate that Focused Shockwave Therapy yields for patients with erectile dysfunction due to lifestyle factors alone — but it certainly helps to speed up the healing process. As an estimate, prostatectomy patients can expect a 20 to 40 per cent success rate for the return of their erectile function with Focused Shockwave Therapy.

How do you help patients to manage bladder incontinence post-op?
To help manage incontinence, patients are provided with pants and pads immediately post-op, to be used when their catheter is removed two weeks after surgery. Men can also get a Pacey Cuff urethral control device, if they don't want to rely on pants and pads while they're navigating urinary incontinence. It's a discreet and comfortable device that can be used to prevent urinary leakage, for up to an hour at a time.
We’ll see patients again two weeks post-op, once they’ve had their catheter removed. It’s a good time for them to come in because at this stage in their recovery, they’ll still be wearing pads.
Our aim is to get men completely dry as soon as possible. Being in pants and pads can feel humiliating for a lot of men, even stopping them from going out and wanting to socialise.
We follow a nine-step pad weaning protocol. In the first instance, we ask patients to keep a diary of what they’re drinking — lots of things can be irritants for the bladder, like tea, coffee and alcohol — and how often they're drinking, particularly as large volumes of fluid can be difficult for the bladder to take. It's also useful for them to keep a tally of the number of pads they’re using per day.
They can then start slowly weaning themselves off – from discarding pads at nighttime if they have three dry nights in a row, to delaying application in the morning. They should keep working on their pelvic floor to enable them to go longer and longer without pads, increasing the gap between use.
By stage five, men should only need a pad if out, exercising or at work; stage six is no longer using pads in the evenings or mornings at home as well.
Stage seven is only using a pad if you’re out or drinking alcohol, at special occasions like weddings; stage eight is when they only need to have a pad in their pocket for emergencies. After this, the next and final stage is forgetting pads all together, because your pelvic floor is working like a dream, and you know you’ll be able to hold it until you make it to the toilet.
Also, it's not often talked about but, because the surgeon removes a portion of the urethra, the surgery shortens the penis.
What kind of support is out there for prostate cancer patients, to help them manage pre- and post-surgery?
Patients have a urology nurse who will help to guide them and refer them to the appropriate services, regarding post-operative rehab.
Medication can be prescribed to help men get their erections back. A dose of 5mg of Cialis or Tadalafil per day is optimum to assist in the recovery following prostatectomy and is a good step towards regaining erectile function. Another option is to get Caverject penile injections to stimulate erections.
For patients wishing to regain their erectile function, their surgeon, urologist or GP can refer them to a penile pump clinic where they can get a pump on prescription to help them restore their erections. The pump is a vacuum device that they can start using around eight to 12 weeks post-surgery, to help get the maintenance erections that the penis needs to remain healthy. The penis needs a flush of healthy, oxygenated blood and tissue expansion to maintain length and girth and using the pump offers a replacement for the maintenance nocturnal and morning erections.
And of course, it's important to get back to exercising — strength training is great for testosterone production and cardiovascular activities are important for vasodilation and the creation of nitric oxide. Beetroot juice is also a great supplement to help with nitric oxide production.




















